Is mealtime a constant battle in your home? Does your child refuse to eat most foods or gag when trying something new?
You’re not alone. Many children face eating difficulties during their early years. While some kids grow out of picky eating, others need extra help to develop healthy eating habits.
Food therapy for kids can make a real difference. It’s a specialized approach that helps children overcome physical, sensory, and behavioral challenges around eating.
This guide will help you understand what feeding therapy is and how it works. You’ll learn the clear signs your child may need professional support. We’ll also share practical tips to make mealtimes easier for everyone.
If you’ve been worried about your child’s eating, this information can help you move toward happier mealtimes.
What Is Food Therapy for Kids?
Food therapy is a specialized treatment that helps children develop healthy eating patterns. Trained professionals work with babies, toddlers, and older kids who struggle with eating.
These professionals include:
- Occupational therapists
- Speech-language pathologists
- Pediatric feeding specialists
This therapy goes beyond just teaching a child to eat. The main goal is to make eating physically easier. It also aims to make mealtimes mentally less stressful for the whole family.
According to the American Speech-Language-Hearing Association (ASHA), feeding and swallowing problems are common in childhood. Early treatment leads to better outcomes.
Kids can be picky eaters. But some children face deeper challenges that don’t go away on their own. These include:
- Difficulty chewing or swallowing food safely
- Strong reactions to certain textures or temperatures
- Extreme anxiety around mealtimes
- Refusing entire food groups for months
Therapists identify each child’s specific difficulty. This could be extreme pickiness or physical limitations like trouble coordinating muscles needed for eating.
Types of Feeding Therapy Approaches
Not all feeding therapy looks the same. Therapists use different methods based on your child’s needs. Here are the most common approaches.
1. Medical-Based Feeding Therapy
This type focuses on underlying health conditions that affect eating. It addresses issues like:
- Swallowing disorders (dysphagia)
- Acid reflux or GERD
- Structural problems in the mouth or throat
- Neurological conditions affecting eating
Children with conditions like cerebral palsy or Down syndrome often benefit from this approach.
2. Sensory/Oral Motor-Based Therapy
This approach targets sensory sensitivities and muscle coordination. It helps children who:
- Gag at certain textures
- Have weak jaw or tongue muscles
- Struggle to chew properly
- React strongly to food smells or temperatures
3. The SOS Approach (Sequential Oral Sensory)
Dr. Kay Toomey developed this popular method. It encourages children to explore food using all their senses. Kids don’t have to eat right away.
The steps include:
- Looking at the food
- Interacting with it (using utensils)
- Smelling it
- Touching it with fingers, hands, then the mouth
- Tasting with the tongue
- Biting and spitting out
- Chewing and swallowing
This low-pressure approach reduces anxiety around new foods.
4. Get Permission Approach
This child-led method builds trust between caregiver and child. The therapist reads cues from the child. They only move forward when the child “gives permission.”
This works well for children with trauma around eating or severe food anxiety.
5. Beckman Oral Motor Approach
This technique improves muscle control in the lips, jaw, tongue, and cheeks. It helps children who struggle with the physical act of eating.
Therapists guide children through specific movements. These build strength and coordination for chewing and swallowing.
6. Behavioral Approaches
These use positive reinforcement to encourage new eating behaviors. Therapists create routines and reward systems. Over time, children try new foods without needing rewards.
Learn more about pediatric feeding disorders from Feeding Matters, a nonprofit dedicated to this issue.
How Food Therapy Works?
Food therapy begins with understanding your child’s specific challenges. The process is structured to address both the physical and emotional aspects of eating.
1. Evaluation and Assessment
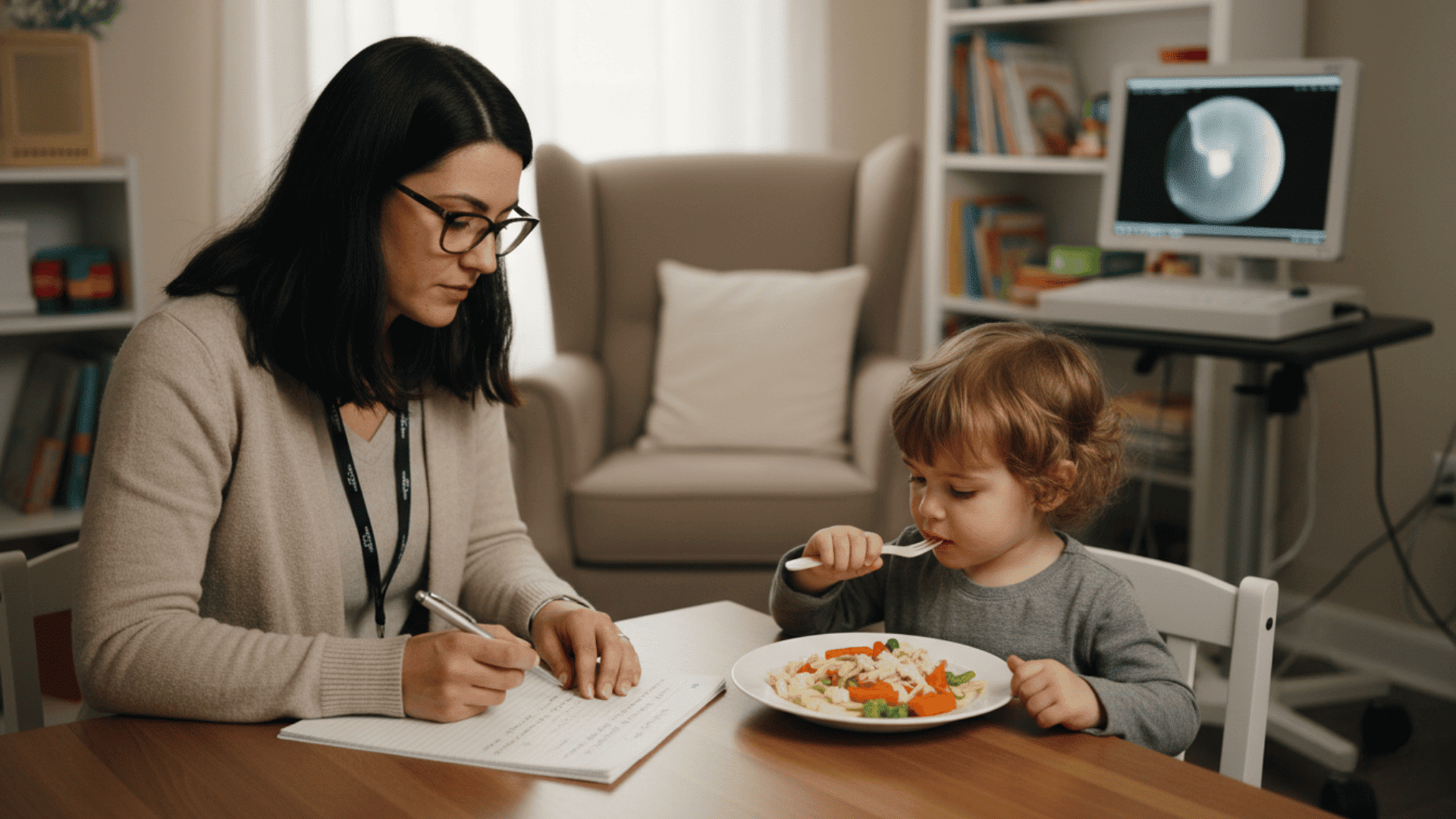
The first step is a complete feeding evaluation. This helps therapists identify the root cause of your child’s eating difficulties.
During the evaluation, the therapist:
- Gathers your child’s complete feeding history
- Discusses current eating habits and concerns
- Observes your child eating a typical meal
- Checks oral motor skills and swallowing function
- Evaluates sensory responses to different foods
You may need to provide a three-day meal journal. This shows what your child eats during normal days at home. Some children also need a swallow study. This checks if they can swallow safely.
Based on the evaluation, the therapist creates a custom plan. This plan includes:
- Specific therapy techniques to use
- Goals for improving eating skills
- Strategies for introducing new foods
- Recommendations for home practice
- Timeline for checking progress
2. Techniques Used in Therapy

Sessions typically last 30 to 60 minutes. They happen once or twice a week. The frequency depends on your child’s needs.
Each session follows a structured format:
Warm-Up (5-10 minutes): Activities prepare your child’s mouth for eating. These might include blowing bubbles, tongue exercises, or cheek puffing.
Feeding Practice (15-30 minutes): The main part focuses on building specific skills. Your child might work on trying new foods. They might improve chewing or learn to use utensils.
Food Exploration (10-15 minutes): Many therapists use play-based learning. Your child explores foods through touch and smell. There’s no pressure to eat. This builds curiosity and reduces fear.
Progress Review (5-10 minutes): The therapist discusses what happened during the session. They answer your questions. They give you strategies to practice at home.
3. Family Involvement
Parents play a vital role in feeding therapy. You are part of your child’s care team.
Therapists stay in close contact with families between appointments. They teach you the same strategies used in sessions. This helps your child practice new skills every day.
The therapy only works if skills transfer to the home. Since sessions happen once or twice a week, daily practice makes the real difference.
Understanding how therapy works helps you feel prepared for the process ahead. But how do you know if your child actually needs this kind of help?
Feeding Therapy by Age Group

Therapy looks different depending on your child’s age. Here’s what to expect at each stage.
Infant Feeding Therapy (0-12 Months)
For babies, therapy often addresses:
- Latching difficulties during breastfeeding
- Problems with bottle feeding
- Coordination of suck-swallow-breathe pattern
- Transitioning from liquids to purees
- Managing reflux during feedings
Therapy for newborns may be more intense. Some babies need multiple short sessions per day. The goal is ensuring proper nutrition during this critical growth period.
Toddler Feeding Therapy (1-3 Years)
Toddlers often struggle with texture transitions. Therapy at this age focuses on:
- Moving from purees to soft solids
- Accepting mixed textures
- Expanding food variety beyond a few items
- Building spoon and cup skills
- Reducing mealtime tantrums
This is a critical window. A 2-year-old’s relationship with food is much easier to change than a 12-year-old’s.
Feeding Therapy for Older Children (4+ Years)
Older children may have years of negative food experiences. Therapy addresses:
- Food anxiety and fear
- Social eating challenges (school lunch, parties)
- Advanced chewing and swallowing skills
- Understanding nutrition basics
- Building confidence around new foods
Cognitive techniques work well with older kids. They can understand and participate in goal-setting.
Signs Your Child Might Need Food Therapy

Most children go through picky eating phases. But some signs point to bigger problems that won’t improve without help.
Knowing these signs helps you decide when to seek professional support. Here are the key indicators broken down by category.
1. Eating Behavior Indicators
Your child refuses to eat or drink consistently. This goes beyond normal pickiness. They might refuse all food for long periods or drink very little throughout the day.
They eat fewer than twenty different foods. Some children will only accept foods from one brand, like only eating chicken nuggets from a specific restaurant.
Mealtimes last longer than thirty minutes for toddlers and young children. The meal feels like a constant struggle with frequent breaks and battles.
Your child shows extreme distress at mealtimes. This includes tantrums, crying, or complete refusal to sit at the table. The anxiety around food affects the whole family.
They suddenly and permanently reject foods they previously enjoyed. These foods don’t come back into their diet even after taking a break from them.
2. Skill and Development Indicators
Your child has trouble chewing age-appropriate foods. They might swallow food in whole pieces instead of chewing it properly or breaking it down first.
They struggle to move from one texture to another. This includes difficulty going from purees to soft solids or from bottle to solid foods at expected ages.
Frequent coughing, gagging, or choking happens during meals. While occasional gagging is normal when learning to eat, consistent problems indicate a physical issue.
Your child can’t use utensils or drink from a cup as expected for their age. Most babies develop a pincer grasp around nine months to pick up small foods.
They pocket food in their cheeks instead of swallowing. This means food stays in the mouth long after they finish chewing, creating a safety concern.
3. Nutrition and Health Indicators
Your child isn’t gaining weight or meeting growth milestones at regular checkups. The pediatrician has expressed concerns about their development falling behind expected ranges.
They avoid entire food groups completely. Refusing all vegetables, proteins, or dairy creates nutritional gaps that can affect their health and energy levels over time.
Your child has specific medical conditions that affect eating. Children with cerebral palsy, autism, Down syndrome, or acid reflux often need specialized feeding support and strategies.
They’re extremely sensitive to food textures, smells, or temperatures. Even being near certain foods can trigger strong reactions like gagging, crying, or leaving the room immediately.
Remember that each child develops at their own pace. But if you notice several of these signs together, it’s time to talk to your pediatrician.
So when exactly should you reach out for professional help? Let’s talk about that next.
When to Seek Professional Help?

Trust your instincts as a parent. If you’re worried about your child’s eating habits, talk to your pediatrician first.
Your doctor can assess whether the eating patterns are typical. They can refer you to a feeding specialist if concerns continue.
Don’t Wait If You Notice Multiple Signs
Some pediatricians may dismiss issues as normal, picky eating. If you disagree, get a second opinion. You know your child best.
Early intervention makes a real difference. Children who receive help sooner tend to progress faster.
Where to Find Help
Look for these professionals trained in feeding disorders:
- Speech-language pathologists (SLPs)
- Occupational therapists (OTs)
- Pediatric dietitians
- Developmental pediatricians
For children under three, contact your state’s early intervention services. Evaluations are often free and include feeding assessments.
You can also search the ASHA ProFind directory for certified feeding specialists in your area.
Questions to Ask a Potential Therapist
Before choosing a feeding therapist, ask:
- What experience do you have with my child’s specific issues?
- Which therapy approaches do you use?
- How do you involve parents in treatment?
- How do you measure progress?
- What is the expected duration of therapy?
What to Expect in Food Therapy Sessions?
Feeding therapy sessions typically last thirty to sixty minutes. They happen once or twice a week, depending on your child’s needs.
Each session follows a structured format designed to help your child feel comfortable and make progress.
Warm-Up Activities: Sessions start with activities that prepare your child’s mouth for eating. These might include blowing bubbles, tongue exercises, or cheek puffing to wake up the muscles used during meals.
Feeding Practice: The main part focuses on building specific skills. Your child might work on trying new foods, improving how they chew, or learning to use utensils correctly.
Food Exploration: Many therapists use play-based learning. Your child explores foods through touch and smell without pressure to eat. This builds curiosity and reduces fear around unfamiliar items.
Progress Review: At the end, the therapist discusses what happened during the session. They answer your questions and give you strategies to practice at home between visits.
Family Participation: Some sessions include parents and siblings. This helps everyone learn how to create positive mealtime experiences together.
The therapist tracks development over time and adjusts the plan as your child masters skills. While professional sessions provide expert guidance, what you do at home matters just as much.
Tips for Supporting Your Child at Home

What happens between therapy visits matters for your child’s success. Here are practical ways to reinforce learning during regular meals.
Offer food at the same times each day. Predictable schedules reduce anxiety about when eating will happen. Limit meals to twenty to thirty minutes to prevent exhaustion.
Eat alongside your child whenever possible. Seeing family members enjoy various foods encourages exploration. Invite your child into the kitchen to help with simple tasks like washing produce or stirring batter.
Give choices between two or three options at each meal. Control over decisions reduces resistance. Let them add their favorite dips or sauces to unfamiliar items.
Avoid forcing, bribing, or punishing related to food consumption. These approaches backfire by increasing stress. Remove uneaten items quietly and move on with your day.
Acknowledge any interaction with new items, including touching or smelling. Recognition of small steps motivates continued effort. Understand that improvement happens gradually over weeks and months.
Conclusion
If you’ve made it this far, you’re already doing something important for your child. Recognizing feeding challenges and seeking information shows you care deeply about their well-being.
Food therapy for kids offers real hope. Most children attend sessions once or twice weekly for several months to a year. You may notice small improvements within the first few weeks, though meaningful progress typically takes three to six months.
Remember that feeding difficulties are not your fault. These challenges involve complex physical, sensory, and behavioral factors. With professional support and patience, most feeding issues can improve significantly.
Trust your instincts. If something feels wrong about your child’s eating, talk to your pediatrician about a feeding evaluation. You’re taking the right steps toward happier, healthier mealtimes.